Original Illustration by Katie Lawliss, Psy.D.
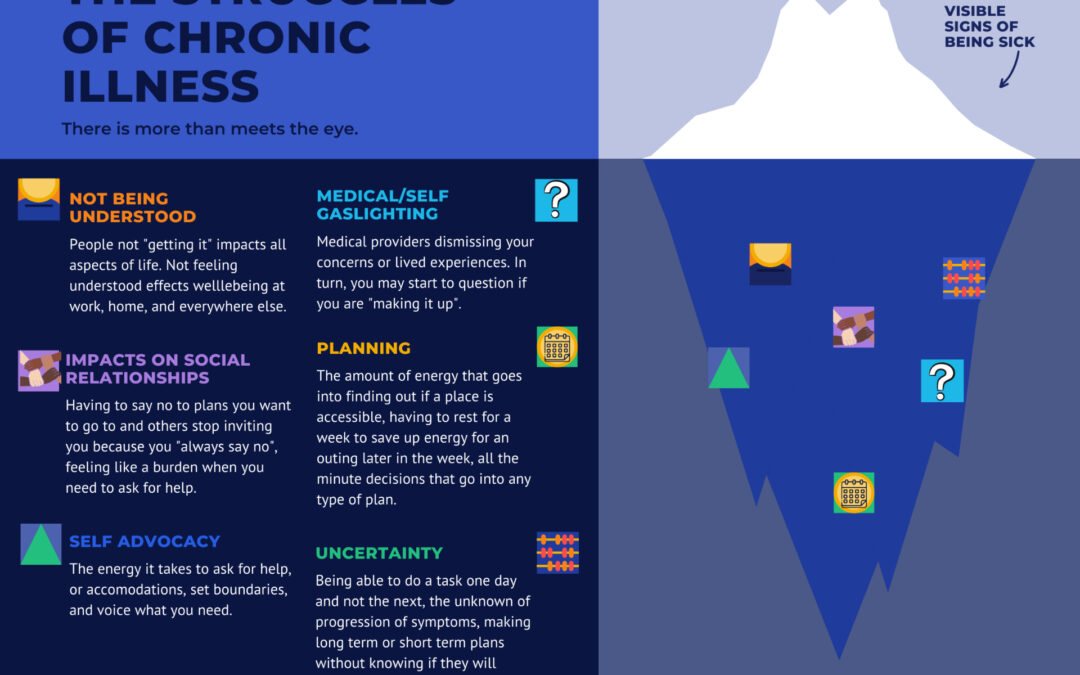
There are so many parts of having a chronic illness that impact emotional wellbeing. Here are just a few:
Struggle #1: Not Being Understood
Someone without your condition may know what they read about it on Google. Some may do more research and work to understand how your condition affects you specifically. However, living with a chronic illness is different than knowing about it. Oftentimes, feeling like others cannot understand what you go through on a day to day basis can feel isolating, sad, and frustrating.
To help cope with this, a phrase I often use is, “What a privilege it is to not understand chronic illness.” The people in your life are lucky to not have the insider scoop on what it’s like to be sick all the time. That does not mean it isn’t painful when the people you love don’t understand your struggles. It also doesn’t mean it’s okay for them to invalidate your experiences and not make an effort to understand as best as they can.
Coping Strategy: Finding an Understanding Community.
It’s helpful to find a community of people (online or in person if your condition allows for that), who can understand what it’s like to live with a chronic illness. This can be people who have the same chronic condition or people who have a general chronic health issues that you can relate to on some levels. Additionally, sometimes following social media accounts can be helpful to know you are not alone in your struggles. Some accounts to check out on Instagram include: @thechroniccommunity, @fourmorespoons, and @how.u.feeling.
Struggle #2: Impacts on Social Relationships
Another difficult part of having a chronic illness is how it affects each relationship in your life. For example, there can be many times you make plans with friends and family and then need to cancel them because you don’t feel well. This is hard for a few reasons. Firstly, it can be hard because you may have been really excited to go do something and then can’t go, either because you don’t feel well, or because you feel that going would be bad for your health. Consequently, perhaps the disappointment that you feel is strong when this happens.
Although you may have loved ones who understand your situation, it can still be hard to see their disappointment when you can’t attend something they were hoping you could. Additionally, those who don’t know you as well or are not as understanding of your condition may express negative feelings about how you are “flakey” without realizing how badly you wish you could follow through on plans. Ultimately, these cancelations may then lead to not being included in plans as often because people assume you will not be able to attend anyway. All of these outcomes hurt in their own way and impact social relationships.
Coping Strategies: Transparency and Self-Compassion
It’s important to communicate with others as well as yourself. It may feel difficult to be open about how your illness affects your ability to make and stick to plans, but allowing yourself to be vulnerable and have these conversations can help your friends and family understand more. They will then be able to understand that you still want to be invited even if you are not sure if you will be able to attend.
Likewise, it’s also important to practice self-compassion. It’s hard to be sick and it’s hard to see it affect your relationships. Remind yourself of this and give yourself some love.
Struggle #3: Medical- and Self-Gaslighting
Unfortunately, many people with chronic illness spend years trying to figure out their diagnosis. Some may know their diagnosis, but be told their symptoms don’t match up with it and, therefore, must be related to anxiety or depression instead. Oftentimes, people hear that so often from multiple sources that they start to question themselves and wonder if they are making it all up. Having your lived experiences be dismissed or not believed is harmful and takes a toll on your wellbeing.
Coping Strategy: Self-Validation
To avoid second guessing yourself, work on validating yourself. You can use affirmations such as, “I know my body better than anyone else;” “I know I don’t feel well even if others don’t believe me;” and, “I deserve someone to believe me.” Additionally, while it does take extra energy, it’s okay to seek second or third opinions, to ask as many questions as you need to, to your providers, and to end a relationship with a provider who invalidates your concerns. Remember that you are your own independent person and are allowed to make your own choices about your health.
Struggle #4: Self-Advocacy
Frustratingly, self-advocacy is crucial in chronic illness, and it’s exhausting! There is a burden to having to advocate for yourself on a consistent basis to providers, friends, family, employers, and more. While it’s important to do, as mentioned above, it’s also hard to do especially when in pain and exhausted.
Coping Strategies: Preparing a Script and Asking for Help
To ease the burden of constant and possibly repetitive self-advocacy, you can write out a gist of your circumstances and needs and re-use it in different settings so you do not need to reinvent the wheel each time you need to advocate for yourself. You can also ask your friends or family members to advocate for you when you need a break from doing it yourself. Remember: it’FFs good to remind yourself that you are worth advocating for.
Struggle #5: Planning
Furthermore, there’s a ton of planning required when it comes to having a chronic illness. “The Spoon Theory” by Christine Miserandino discusses how chronic illness requires planning due to fatigue and pain. If someone wants to go to their best friend’s birthday party, they need to account for energy expenditure for each “small” task for the week in advance, including, decisions about when to expend energy on showering, preparing food, and more. You can read more on “The Spoon Theory” here. I encourage you to read the article and use it to give yourself credit for all you do and to use the language when explaining chronic illness to people in your life..
Additionally, outside of planning for energy expenditure, you likely are managing planning medical appointments and keeping up with prescriptions, which includes going to the pharmacy, keeping track of what you are low on, making sure your doctors have sent in prior authorizations for medications, and the dreaded long phone calls with both insurance companies and mail order pharmacies. These are just two of the many logistical planning tasks required of having a chronic illness.
Coping Strategy: Organization Tools
Using systems that work for you including setting reminders on your phone, keeping a planner, and enlisting the help of a loved one can help with this burden.
Struggle# 6: Uncertainty
Lastly, in addition to all of the struggles above (and more that are not listed) there is the heavy weight of uncertainty when having a chronic illness. Life is not certain for anyone, but with chronic illness you are faced with a tremendous amount of uncertainty. Chronic illness affects everything in life so you live every day not knowing what your symptoms will be like tomorrow, next week, or a year from now. You may not know the prognosis of your condition, or maybe you know the statistics but are not sure where you fit into the statistics. On top of that, you may not know what treatments will help, which will have side effects, and which treatments don’t exist yet but could be life changing. These are just a few examples of the many ways in which chronic illness is uncertain.
Coping Strategy: Keep Pursuing Your Passions
Coping with uncertainty is difficult and it requires you to think about what matters most to you. Reflect on what gives your life meaning and do things that are in line with that. Perhaps you love helping animals and when you were young you wanted to open an animal sanctuary, maybe that would be too much for your body now; however, you could volunteer at a shelter once a week or once a month. Alternatively, maybe social justice is important to you and you can’t be on the front lines of a protest, but you can make phone calls or send mailers to encourage people to vote.
You can still pursue long term goals and exist with the discomfort of not knowing what the end result will be. It’s still worth engaging in these goals even if it’s not exactly how you originally pictured it. Pursue a degree if that is important to you, start the business you want, or volunteer for something you are passionate about! It’s okay to do these things even if you don’t know how long you will do them for or what it will look like. Contrastingly, it’s also okay to grieve. Living with a chronic illness includes grief, especially when it comes to uncertainty.
In conclusion, coping with chronic illness looks different for everybody but I hope you can give yourself credit for all you do, even when others don’t understand. I hope you allow yourself to grieve. More importantly, I hope you find a way to live a meaningful life even if it looks different than what you planned or what you see others doing.